Clonus Explained: What It Is, Why It Happens, and What You Can Do About It
Stop Letting Leg Cramps Slow Your Recovery
Can Clonus Affect the Way You Walk? Absolutely—Here’s What You Need to Know
Have you ever felt your foot suddenly jerk, cramp, or bounce when you’re walking or standing?
It can be surprising, frustrating, and even a little scary. If this sounds familiar, you might be dealing with clonus—a common but often misunderstood movement issue after a stroke or other neurological injury. But understanding what’s going on in your body is the first step toward finding solutions.
In this post, we’ll break down what clonus is, how it impacts walking, and what you can do to reduce its effects.
What is Clonus?
Clonus is a series of involuntary, rhythmic muscle contractions—basically, your muscles start moving on their own without you telling them to. It usually happens when there’s been damage to the brain or spinal cord, particularly the areas that control movement.
A common way clonus is triggered is by quickly flexing your foot upward. For many stroke survivors, this can happen without meaning to, especially when the foot lands slightly pointed or toe-first.
How Does Clonus Affect Walking?
For some, clonus can feel like a cramp or sudden spasm. When the foot hits the ground even slightly pointed, the reaction causes it to bounce or point rapidly.
This reaction may cause you to avoid putting weight on that leg which can create a number of walking challenges.
Let’s break down a few common ways clonus shows up in walking and why it happens:
1. Swinging the leg out to the side (Abducted gait)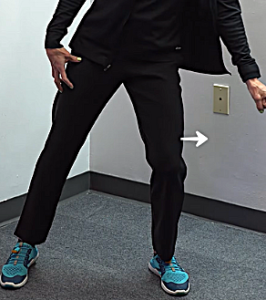
If clonus kicks in when you step, you may start avoiding that leg altogether. This might look like swinging your leg out to the side or quickly shifting your weight to the other leg to avoid the spasm. Over time, this can throw off your balance and cause other parts of your body to compensate
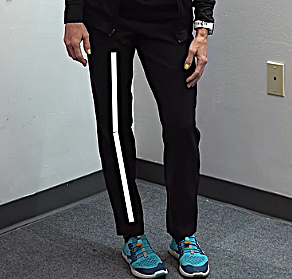
2. Step-To Walking Pattern
Instead of taking a full step-through with the affected leg, you may find yourself bringing your other foot next to it—kind of like walking in short shuffles. This is often your body’s way of minimizing movement in the leg that triggers clonus, but it makes walking less fluid and more tiring.
 3. Knee hyperextension (locking the knee back) when the foot (“toe first”) hits the ground
3. Knee hyperextension (locking the knee back) when the foot (“toe first”) hits the ground
When your foot hits the ground toe-first, it can suddenly snap upward (called dorsiflexion), triggering clonus. This quick movement causes your calf to tighten and may force your knee to lock backward. Over time, this puts stress on your knee and increases your risk of joint pain or falls.
4. Feeling like you’re falling backward as the foot reacts by pointing and throwing off your balance.
That sudden jerky movement in your foot can make it hard to shift your weight forward. As a result, you may feel like you’re going to fall backward, especially when trying to walk faster or go up a slope. This can make you hesitant to walk, which slows down progress.
What Can Help?
AFO (Ankle-Foot Orthosis):
-
-
-
Wearing a properly fitted AFO can prevent your foot from landing toe-first, which helps stop clonus from kicking in.
-
If your foot stays pointed down and you don’t have enough active movement to lift it, an AFO can help protect your knee and improve your walking pattern.
-
If you don’t have at least 10 degrees of foot lift (dorsiflexion), you should be wearing an AFO.
- A heel wedge helps avoid quick stretch if the foot is slightly pointed.
-
-
Calf Stretching: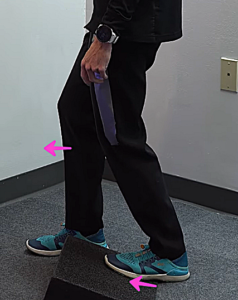
-
-
-
Stretching your calf can help the ankle move better and reduce the quick stretch that triggers clonus.
-
Aim to stretch enough so your ankle can bend up to at least 10 degrees.
-
-
Jumping:
-
-
-
-
Controlled jumping helps your ankle get used to fast movements.
-
It won’t get rid of clonus completely, but it can help your body get more comfortable and reduce how much it affects your walking.
-
-
-
Conclusion
Clonus can be frustrating, especially when it interferes with walking and everyday movement. But understanding what’s happening—and why—is the first step to taking back control. Whether it’s finding the right brace, improving ankle flexibility, or training your body to handle different speeds, small adjustments can go a long way. Progress may not always be quick, but every step you take is part of your comeback.
Articles you may be interested in
How to Fix An Abducted Gait
Reclaim Your Stride: Fixing Abducted Gait After Stroke https://youtu.be/VGvg5qeLmy0 Recovering from a neurological injury can affect your walking pattern, one of which is the "abducted leg walking pattern." In this post, we'll cover what it is, its causes, and how to...
How to Fix a Trendelenburg Gait
Why Your Hip Drops When You Walk : How to Regain Stability https://youtu.be/37akItHE9mcHave you ever noticed that one side of your hip drops lower when you walk? Maybe someone pointed it out, or you feel off-balance or unsteady when taking steps. This could be a sign...
Correct Knee Hyperextension after a Neurologic Injury
Struggling with Knee Hyperextension? Here's How to Fix It! Does your knee snap backward when you walk? Do your steps feel jerky, unsteady, or inefficient? If so, you might be dealing with knee hyperextension, a common issue after a stroke, brain injury, or...
How to Fix a Vaulting Gait
How to Stop Vaulting and Walk More Naturally After a Stroke If you’ve ever noticed yourself pushing up on your stronger leg to swing your weaker leg forward while walking, you may be experiencing vaulting. The good news? Vaulting can be unlearned with the right...
Discover 15 Principles to Rewiring Your Brain Faster
Discover 15 Principles to Rewiring your Brain Faster Transform Your Mindset and Achieve Rapid Results https://youtu.be/rfSCk_qJe64 Neuroplasticity: Your Brain’s Superpower After a stroke, the brain can suffer damage, but it’s far from the end. But here’s the good...
Eye Exercises for Stroke Survivors: Regaining Vision and Function
Visual impairment is a very common consequence in stroke survivors—almost 50% of stroke survivors become visually impaired. This is primarily because the brain's visual pathways are blocked or damaged when a person experiences a stroke. As a result, patients often...
Discharged from therapy. What now?
So, you have been discharged from therapy. So, what now? For some, this is a positive step in the rehab process. Some will understand right away that this is progress. On the other hand, for others it can bring up all kinds of negative emotions. "Is my therapist mad...
Hemineglect after a stroke: When half the world is missing
hemineglect is a condition where someone loses the ability to attend to, sense, and/or perceive information on one side. This condition is also referred to as unilateral neglect, spatial neglect, and/or hemispatial neglect. Several neurologic condition can cause this...
Post Stroke Pain: Diagnosis and Treatment
Pain is a common symptom after a stroke. Unfortunately, pain can be a significant barrier to regaining function. In some cases, there is an identifiable cause related to a movement or a structural problem. The rehab team can identify this, prescribe the...
Brunnstrom Stages of Motor Recovery
The Brunnstrom stages of stroke recovery is one proposed model of how someone with hemiplegia will recover movement. It was developed by a physical therapist in the 1960s and proposes that this sequence of recovery falls into six loosely defined stages. The main...













