Pain is a common symptom after a stroke. Unfortunately, pain can be a significant barrier to regaining function. In some cases, there is an identifiable cause related to a movement or a structural problem. The rehab team can identify this, prescribe the appropriate exercises, and voila…….problem solved. But what if that is not the case? What if your pain seems to come out of nowhere? There are two post stroke pain conditions that do just that. They are central post stroke pain and complex regional pain syndrome.
What is Nociceptive pain?
Nociceptive pain is a distressing feeling often times caused by a noxious stimulus. A noxious stimulus is a potentially tissue damaging event. A noxious stimulus can be mechanical (causing structural damage to tissue), chemical (the bodies exposure to an acid or irritant), and/or thermal (exposure to extreme and potentially damaging heat or cold).
Nociceptive pain is meant to draw a person’s attention to that area of the body to:
- Prompt a person to withdraw from a potentially damaging situation
- Protect an injured body part while it heals
- Avoid similar situations in the future
Ideally, once the potentially damaging stimulus is removed or that area of the body has healed, the pain subsides.
What is neuropathic pain?
Neuropathic pain on the other hand is an unpleasant sensation is caused by damage or a breakdown in the nervous system. Neuropathic pain develops without any type of an external noxious stimulus.
What is post stroke pain?
Unfortunately post stroke pain is complicated. Rarely, does pain after a stroke fit the a+b=c model of nociceptive pain. Post stroke pain is more of a combination of nociceptive and neuropathic pain. I have written extensively on the many structural and movement problems that can happen after a stroke. And yes, abnormal movement and/or structural deformities can lead to nociceptive pain. However, neuropathic pain is all to common. Two of the most common neuropathic pain conditions is central post stroke pain and complex regional pain syndrome.
What is Central Post Stroke Pain?
Central post stroke pain is a type of pain that originates in the brain. The uncomfortable sensation is due to a lesion in one of the brain’s “pain centers”. This feeling is often described as throbbing, burning, stabbing, tingling, aching, or shooting pain. As the name suggests, there is no identifiable stimulus in the periphery that would warrant this type of sensation. Hence the name central post stroke pain.
Symptoms of CPSP can be induced or spontaneous. Induced pain is an increase in sensitivity to a stimulus that would not be considered painful under “normal conditions”. For example, the same touch on the involved arm and the uninvolved arm may be perceived as painful only on involved arm. Spontaneous pain develops independent of any stimulus. This type of pain may be continuous or intermittent.
The exact mechanism of CPSP is poorly understood. That being said, diagnosing CPSP is usually through process of elimination. In other words, a doctor may rule out every other possible cause prior to settling on CPSP as the diagnosis.
What is the treatment for CPSP?
Several groups of medications have been shown to be effective in treating CPSP.
Anticonvulsants – Many antiepileptic drugs have been proven effective in treating CPSP. Calcium channel modulators such as gabapentin and pregabalin are also commonly prescribed.
Anti-depressants – Selective Serotonin reuptake inhibitors (SSRI) have been used however there is limited data that shows a clinically significant change in a patient’s report of pain.
It is important to note that these medications have severe a dangerous side effects and therefore finding the correct medical doctor to diagnose and treat CPSP is critical. A physiatrist (physical medicine and rehab doctor) typically has the best understanding of this condition and should be considered.
It is also important to note that there is a consensus amongst the literature that CPSP has been linked to the opioid receptors in the brain. The studies have shown that there is decreased binding of the opioid receptors. The claim is that opioids may actually make CPSP pain worse. And in fact, this has been my experience when working with patients. That being said, it is extremely important to find a doctor who understands CPSP in an effort to prescribe the appropriate medications for this pain condition.
What is complex regional pain syndrome?
Complex regional pain syndrome (CRPS) is often called shoulder hand syndrome when it occurs following a stroke. CRPS is characterized by:
- Burning pain
- Hypersensitivity to light touch
- Edema (swelling) in the hand or lower leg
- Change in skin temperature
- Change in skin color
Different from central post stroke pain, CRPS is rarely linked to a specific “type” of stroke or the location of a lesion in the brain. However, there are certain risk factors that might predispose someone who has suffered a stroke with developing this condition:
- A flaccid arm
- Shoulder subluxation
- “Poorer”or lack of functional recovery
What is the mechanism that causes complex regional pain syndrome?
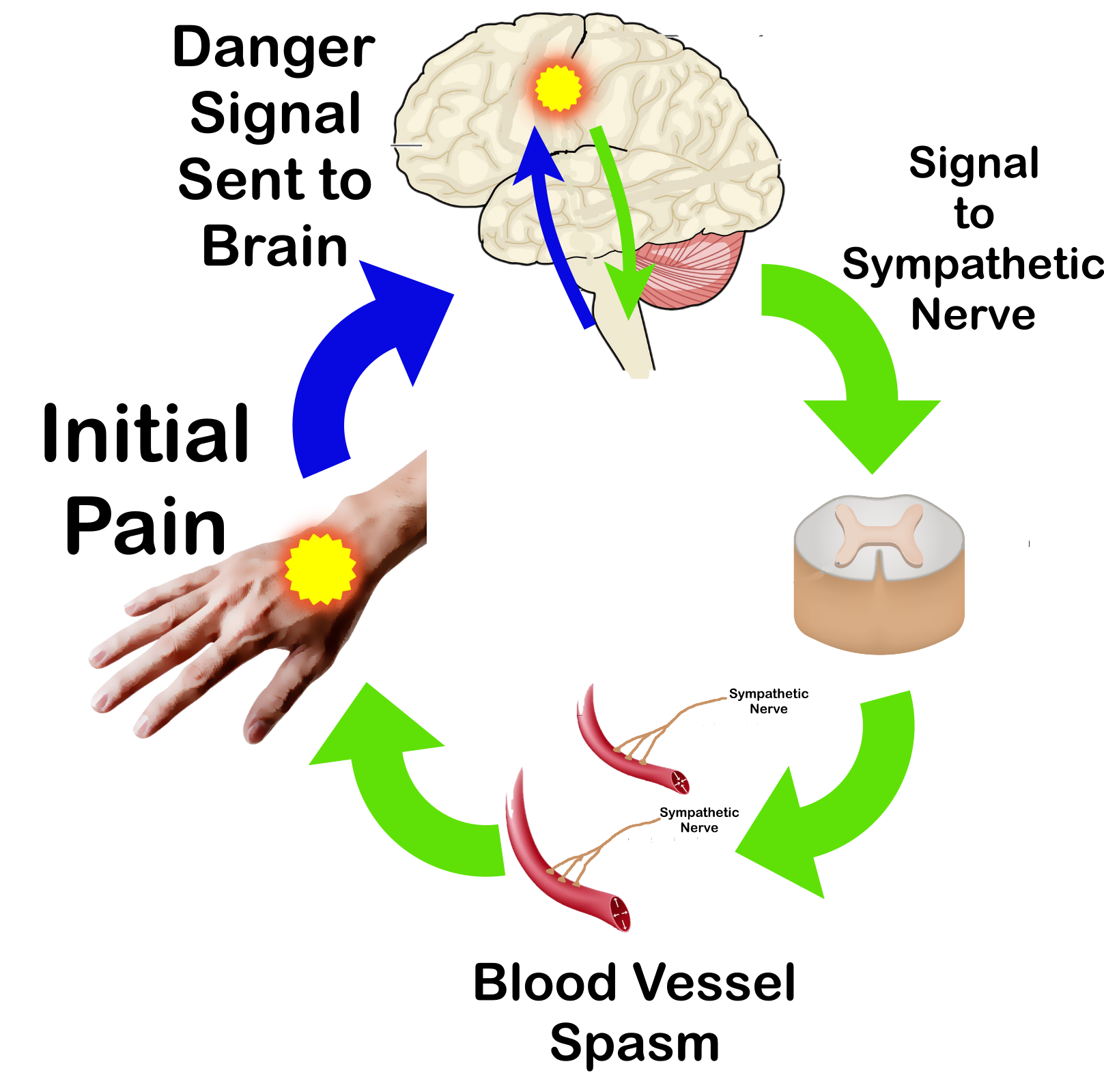
CRPS pain occurs due an overactive sympathetic nervous system. The sympathetic nervous system is responsible for directing the bodies rapid involuntary response to a stressful or dangerous situation. This is often referred to as the “flight or fight” response and is characterized by increased alertness and heart rate, and by sending increased blood to the muscles due to a blood vessel spasm. Hence the swelling that is often times found with this condition.
The difference of CRPS compared to CPSP is that there is typically an initial trigger to the pain.
Complex Regional Pain Syndrome Treatment
The best way to NOT experience complex regional pain syndrome is prevention. Early mobility and protecting the shoulder from injury are two ways to prevent this type of abnormal pain response. Once you have developed this condition, you still want to perform passive range of motion exercises and continue to keep the shoulder positioned to prevent injury or prevent a painful “trigger”. Other treatments interventions include:
Desensitization – Starting with light touch with a very soft material such as a cotton ball. As the body gets used to this and does not trigger any type of a pain response, progress to a more abrasive material such as a cotton shirt. Continue to progress to a denim material and finally something very abrasive such as a dish sponge. You can also try things such as sticking the hand in sand or rice to introduce other textures.
Mirror Therapy – Mirror therapy uses a mirror box to reflect the uninvolved arm which has been known to effectively treat a variety of pain conditions.
Medication – Work with a physiatrist (physical medicine and rehab doctor). Keep in mind, this might be a trial and error method to settle on an effective medication so be patient.

