How to Stop Vaulting and Walk More Naturally After a Stroke
If you’ve ever noticed yourself pushing up on your stronger leg to swing your weaker leg forward while walking, you may be experiencing vaulting.
The good news? Vaulting can be unlearned with the right strategies.
In this post, we’ll explain what causes vaulting, why it happens, and the simple exercises you can do every day to improve your walking pattern.
What is Vaulting?
Vaulting happens when you rise up on your uninvolved leg to help swing your involved leg through. It may seem like a quick fix, but it actually increases energy use, imbalance, and joint strain, making walking more tiring and less stable.
Vaulting is a learned habit, meaning with consistent training and adjustments, you can retrain your body to walk more naturally.
Why Does Vaulting Happen?
There are several reasons why you might develop a vaulting gait pattern:
1. Your leg is longer or your brain is perceiving it as longer
If your brain perceives your involved leg as longer or it is physically longer, you may vault to help clear the foot.
Possible Causes: If your AFO (brace) is pointing downward or your calf muscles are tight, your foot might not clear the ground properly, making it feel like your leg is longer.
Treatment:
✔️ Adjust your AFO by removing the heel wedge at the bottom of your brace.
✔️ Raise the other shoe by wearing one with a slightly thicker sole.
✔️ Stretch your ankle regularly to improve flexibility and movement.
2. Spasticity
If your quadriceps (thigh muscles) are tight, your knee may stay locked straight, making it hard to swing your leg forward normally.
Treatment:
✔️Work on stretching and relaxing tight muscles to allow for better movement.
3. Your Brain Won’t Let Your Leg Bend (Inability to Dissociate)
This happens when legs are unable to perform different movements at the same time.
For example:
- When you’re standing on one leg, the other leg won’t bend as it should.
- If you try to bend one leg, the opposite leg may bend too, instead of moving separately.
Sometimes, when you stand on one leg, your brain doesn’t allow the other leg to bend out of fear it will buckle. Instead, it keeps both legs straight, making walking harder.
Treatment:
✔️ Balance exercises and movement retraining can help correct this pattern.
4. Weakness in Hip flexors
If your hip flexors are weak, you may not have enough strength to lift your leg forward without compensating.
Treatment:
✔️Strengthening exercises to improve hip flexor activation.
How to Fix Vaulting – 3 Simple Exercises
The key to breaking the habit of vaulting is consistent practice. Here are three exercises to help you retrain your gait:
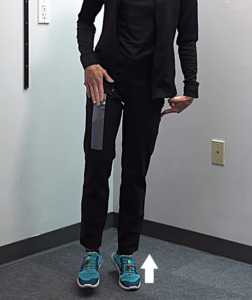
1️⃣Even-Up Shoe
– Wearing a slightly thicker sole on the other foot can help make walking feel more balanced, so you won’t feel the need to push up on your toes.
2️⃣Crouch Walking
– Walk with slightly bent knees while keeping your hands behind your back, and take small steps. This encourages proper movement and prevents vaulting.
- Try to keep your hands behind your back.
- Bend both knees.
- Take small steps.
3️⃣Resistance Band Hip Flexion 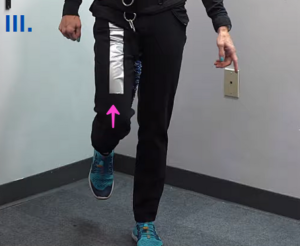
– Use a resistance band to help lift your knee and hip repeatedly. This strengthens the muscles needed to clear your foot properly.
Conclusion
Vaulting may feel like a natural way to get your leg through when walking, but over time, it can lead to inefficiency, imbalance, and extra fatigue. The good news? With simple daily exercises and adjustments, you can retrain your brain and body to move more naturally.
Recovery takes patience and consistency, but every small change brings you one step closer to better, smoother walking. Stay patient, keep practicing, and trust the process—you’re making progress with every step!
Articles you may be interested in
The Pain-Avoidant Loop After Stroke: How Pain Can Stall Recovery
The Pain-Avoidant Loop After Stroke: How Pain Can Stall Recovery Pain after a stroke is real.It can be sharp, nagging, constant, or unpredictable.And it has a sneaky way of slowing down recovery in ways many people don’t realize. This is what I call the pain-avoidant...
The Cycle of Learned Non-Use
The Cycle of Learned Non-Use In the early days after a stroke, attempts to move the affected arm often fail or are painful. Naturally, the brain (and the person) adapts by relying more on the stronger, unaffected side. The result? The brain starts to “forget” the...
How to Fix An Abducted Gait
Reclaim Your Stride: Fixing Abducted Gait After Stroke https://youtu.be/VGvg5qeLmy0 Recovering from a neurological injury can affect your walking pattern, one of which is the "abducted leg walking pattern." In this post, we'll cover what it is, its causes, and how to...
How to Fix a Trendelenburg Gait
Why Your Hip Drops When You Walk : How to Regain Stability https://youtu.be/37akItHE9mcHave you ever noticed that one side of your hip drops lower when you walk? Maybe someone pointed it out, or you feel off-balance or unsteady when taking steps. This could be a sign...
Correct Knee Hyperextension after a Neurologic Injury
Struggling with Knee Hyperextension? Here's How to Fix It! Does your knee snap backward when you walk? Do your steps feel jerky, unsteady, or inefficient? If so, you might be dealing with knee hyperextension, a common issue after a stroke, brain injury, or...
Discover 15 Principles to Rewiring Your Brain Faster
Discover 15 Principles to Rewiring your Brain Faster Transform Your Mindset and Achieve Rapid Results https://youtu.be/rfSCk_qJe64 Neuroplasticity: Your Brain’s Superpower After a stroke, the brain can suffer damage, but it’s far from the end. But here’s the good...
Eye Exercises for Stroke Survivors: Regaining Vision and Function
Visual impairment is a very common consequence in stroke survivors—almost 50% of stroke survivors become visually impaired. This is primarily because the brain's visual pathways are blocked or damaged when a person experiences a stroke. As a result, patients often...
Discharged from therapy. What now?
So, you have been discharged from therapy. So, what now? For some, this is a positive step in the rehab process. Some will understand right away that this is progress. On the other hand, for others it can bring up all kinds of negative emotions. "Is my therapist mad...
Hemineglect after a stroke: When half the world is missing
hemineglect is a condition where someone loses the ability to attend to, sense, and/or perceive information on one side. This condition is also referred to as unilateral neglect, spatial neglect, and/or hemispatial neglect. Several neurologic condition can cause this...
Post Stroke Pain: Diagnosis and Treatment
Pain is a common symptom after a stroke. Unfortunately, pain can be a significant barrier to regaining function. In some cases, there is an identifiable cause related to a movement or a structural problem. The rehab team can identify this, prescribe the...