Hemiplegia (weakness on one side of the body) can be a huge cause of disability following a stroke. This can make activities such as grasping, reaching, and manipulating objects difficult, if not impossible. Constraint Induced Movement Therapy has been well documented to have a positive impact on the quality of arm movement. On the other hand, there is much less convincing evidence that it improves overall disability or burden of care.
All that being said, it is still an extremely valuable treatment strategy with several studies reporting positive brain changes. Therefore, CIMT is definitely one of many tools that should be explored as a potential option as part of stroke rehabilitation program.
What is Constraint-Induced Movement Therapy?
CIMT includes a combination of restraining the uninvolved arm and “forcing” intensive use of the involved (or affected limb). Types of restraints include a standard arm sling, a splint combined with a resting hand splint, or a glove.
History of Constraint-Induced Movement Therapy (CIMT)
The concept that lay the foundation for CIMT was first documented by a German Scientist Munk in 1908. Munk reported that non-human primates would use an impaired arm if forced to do so for a purposeful or meaningful activity.
Several years later, (mid 1960s) this information was utilized to conduct studies with monkeys who had an injury to one hemisphere of the brain. In these later studies the animal’s “better arm” was constrained. As a result, they showed that under these conditions the monkeys would use the impaired arm.
And again in the 1980s this idea re-emerged with the work of Edward Taub, PhD, a behavioral neuroscientist, and his associates. Taub and his associates reported that constraining the involved limb could reverse the effects of “learned non-use”.
What is a standard CIMT protocol?
1. Intensive graded practice with the involved arm with activities aimed at task-specific use for up to six hours a day for two weeks.
2. Immobilizing the uninvolved arm during 90% of the waking hours.
Unfortunately, there are several reasons this protocol is not practical. First, due to insurance limitations and financial constraints, six hours of therapy per day is no possible. Second, asking patients to adhere to a protocol for 90% of their waking hours makes patient compliance (adhering to the protocol outside of therapy) a problem. And, finally, there is some concern for safety. For example, a few studies have reported arm burns caused by an iron.
Due to these factors, a modified CIMT protocol was created and has some moderately convincing evidence that it is equally effective as the traditional CIMT
What is a modified CIMT protocol?
1. Patients attend therapy three days per week for ten weeks where they perform goal-directed activities
2. Patients are asked to wear a mitt on the uninvolved hand for five hours per day (Monday through Friday) for the same ten week period
Compared to traditional CIMT, this protocol is less costly and is easier to implement. However, I have my doubts that the outcome is the same as a the traditional protocol. First, I think the non-compliance is far greater with this protocol. In addition to compliance issues, the dramatic decrease in therapy time make me doubt the claims that his protocol is equally effective.
Why does CIMT work?
Two main reasons why CIMT works.
Neuroplasticity
Neuroplasticity is the brain’s ability to reorganize after injury. One critical component of “brain rewiring” is repetitive practice. Clearly, with the number of hours spent “training” with a (traditional) CIMT protocol, the numbers would speak for themself. In other words, more time practicing will yield more learning. This would be very similar to elite athletes, who also play a “numbers game”. The “Michaels Jordans” and “Kobe Bryants” put in more numbers perfecting their craft to achieve their level of success.
Similarly, CIMT, when compared to “traditional” physical therapy, involves more time “training” each week. Therefore more “learning” and positive brain changes are possible.
Learned Non use
A stroke survivor recognizes early on that it is “too difficult” to use the involved arm and therefore learns ways around that. We call this compensation. Once the brain establishes that there is an easier way, it will take the path of least resistance. This is a form of learned nonuse. And actually you do get neuroplastic changes. Unfortunately the neuroplasticity (rewiring) that occurs actually occurs on the undamaged side of the brain.
Studies of CIMT, if started early, claim that you prevent learned non-use. As learned nonuse becomes more “engrained” into the “hard drive” of the brain, they actually see that the damaged side of the brain is further suppressed. It is important to note that this is different and separate from damage caused by the stroke. These negative changes are seen much later in recovery and therefore are (partially) preventable.
Stroke Recovery and Apathy: What It Is and How to Overcome It
What’s Really Going On When Motivation Disappears After Stroke Recovering from a stroke is a journey that requires strength, patience, and persistence. But for many stroke survivors, the hardest part isn’t weakness, fatigue, or memory loss. It’s something less visible...
Why Your Stroke Exercises Aren’t Helping and How to Fix It
Stroke Recovery Tips: When Exercises Don’t Seem to Work https://youtu.be/9r06T9gtsYc Is it possible to be making progress after a stroke or neurologic injury and still feel like your movement is getting stiffer, heavier or just plain harder?Absolutely. And let me tell...
Struggling with Shoulder Pain After a Stroke? Here’s What Works
Why Does My Shoulder Hurt After a Stroke?Understanding the 6 Most Common Causes and What You Can Actually Do About Them Let’s be real — if you’re recovering from a stroke and your shoulder still hurts, it can feel really defeating. Especially if you’ve been doing “all...
Best Arm Rehab Post Stroke
Discover how new research is changing what’s possible for stroke survivors with little to no arm movement. https://youtu.be/Bw-rd1Fx02cWhat if I told you that even if you can’t move your arm after a stroke, there are still powerful ways to promote recovery—and...
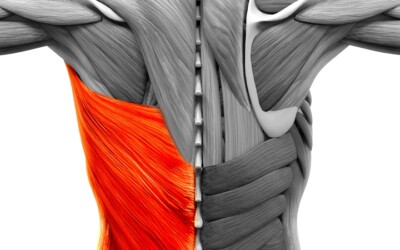
The Hidden Culprit: How the Latissimus Dorsi Limits Shoulder Recovery After Stroke
The Hidden Culprit: How the Latissimus Dorsi Limits Shoulder Recovery after Stroke It’s the silent barrier most people never think about. When we talk about restoring arm movement after a stroke, most of the focus is on the obvious: the shoulder joint, the triceps,...
Why Your Hand Still Won’t Open After Stroke | 3 Mistakes to Fix
Why Forcing It Doesn't Work How to Stop Reinforcing the Wrong Patterns and Start Rewiring Your Brain for Real Recovery https://youtu.be/fDIgGLM8Kj0If you’ve had a stroke (or other neurologic injury), and your hand feels like it’s stuck in a fist or your arm just hangs...
Understanding Abnormal Synergy Patterns After Stroke: The Missing Puzzle Piece in Recovery
Understanding Abnormal Synergy Patterns After Stroke: The Missing Puzzle Piece in Recovery Stroke recovery is rarely straightforward.You might work on strength, balance, and mobility—yet your movements still feel awkward, stiff, or “robotic.” Why?One of the most...
Post-Stroke Shoulder Pain: Why It Happens and What You Can Do About It
Post-Stroke Shoulder Pain: Why It Happens and What You Can Do About It If you’ve had a stroke, chances are your shoulder has tried to steal the spotlight at some point. Not in a good way. Post-stroke shoulder pain is one of the most common (and most frustrating)...
Shoulder Flex by ProStretch: For Improved Shoulder Movement After Stroke
Struggling to stretch your shoulder on your own after a stroke or injury? You’re not alone. External rotation can be one of the hardest movements to work on—especially if your elbow won’t stay in place or one arm isn’t cooperating. That’s exactly why the Shoulder Flex...
Eye Exercises for Stroke Survivors: Regaining Vision and Function
Visual impairment is a very common consequence in stroke survivors—almost 50% of stroke survivors become visually impaired. This is primarily because the brain's visual pathways are blocked or damaged when a person experiences a stroke. As a result, patients often...