Why Does My Shoulder Hurt After a Stroke?
Understanding the 6 Most Common Causes and What You Can Actually Do About Them

Let’s be real — if you’re recovering from a stroke and your shoulder still hurts, it can feel really defeating.
Especially if you’ve been doing “all the things” — exercises, therapy, maybe even injections — and nothing seems to help.
Here’s what I want you to know:
Pain isn’t the problem.
It’s a signal that something needs attention.
So today, I want to walk you through the real reasons your shoulder might still be hurting — and what you can do about it.
Why Medications Alone Don’t Work
Medications may dull the pain, but they won’t fix the cause. Worse, they can delay real treatment. Pain is your body’s signal that something’s off. Covering it up without investigating why it’s there just prolongs the problem.
What’s Actually Causing the Pain?
There are several things that can lead to shoulder pain after a stroke.
But today I want to zoom in on just a few things that I think a lot of you might be missing.
1. Shoulder Subluxation
This is super common after a stroke.
Subluxation basically means your arm bone isn’t sitting fully in the shoulder socket.
And that little “drop” can stretch out soft tissue and cause a ton of pain.
But here’s the tricky part — sometimes you won’t even feel the subluxation.
You’ll just feel pain and not know why.
Try this:
-
- Gentle weight-bearing.

That doesn’t mean a full push-up. It might just mean sitting and leaning gently into your elbow.
That subtle pressure helps push the arm bone back into the socket.
It also gives the shoulder the feedback it needs to relearn how to stay stable.
Start small. Even a few minutes a day makes a difference.
- Positioning
Supporting the arm — especially when sitting or standing — is key.
2. Shoulder Impingement
This one happens when structures inside your shoulder (like tendons or bursa) get pinched —
usually because the shoulder blade or arm bone is in the wrong position.
And here’s the kicker:
You can accidentally cause this if your posture is off, or you’re trying to push through movement without the shoulder blade being supported.
What helps:
Doing movements lying down.
It’s also less effort, so your body stays more relaxed. That helps reduce compensation and spasticity, too.
Avoid pulleys or raising your arm too high until you’ve improved how your shoulder blade moves.
3. Adhesive Capsulitis (Frozen Shoulder)

This is when the joint capsule around your shoulder tightens up — like shrink-wrap. It severely limits how far your shoulder can move and can cause a deep, nagging pain, especially with lifting.
It often sneaks in when the shoulder isn’t being moved enough in all directions, especially external rotation (that out-to-the-side movement you need for things like reaching back into a jacket sleeve).
What helps:
Consistent, gentle stretching — especially external rotation.
This is where I recommend the Shoulder Flex tool. I started using it with clients because it allows a safe, supported stretch into that sticky range. Eventually, I started carrying it in our store because it’s just that helpful.

4. Spasticity
When your brain thinks it needs to work hard, it tightens everything.
You try to lift your arm, and suddenly your shoulder hikes up, your elbow locks, your wrist curls. That’s spasticity.
But here’s the twist:
Sometimes it’s not spasticity.
It’s just your brain trying to help… in all the wrong ways.
What helps:
Active assisted movement.
Especially lying down.
Use your good hand to help the weak arm.
You’ll be less likely to overcompensate. Less spasticity. Better alignment.
And the more your shoulder moves the right way, the more your brain relearns what “normal” feels like.
5. CRPS (Complex Regional Pain Syndrome)
This one’s tough. If you have CRPS, you probably know it’s not just shoulder pain — it’s pain that doesn’t make sense.
Your skin might be sensitive. Light touch might hurt. It feels like your body is on high alert.
What helps:
Progressive exposure to movement.
That means starting with what you can tolerate. Maybe you just rest your hand on a pillow. Maybe you just think about moving it.
There’s no rushing this. But you can retrain the brain to feel safe again.
6. Bursitis or Tendonitis
What it is:
Overuse or poor movement patterns can irritate the shoulder’s tendons or bursae (the cushions between joints).
What it feels like:
Pain that shifts or worsens with activity. It’s often mistaken for other shoulder problems.
What helps:
Reduce inflammation first — rest, ice, gentle motion. Long term, improve how the shoulder moves to avoid flare-ups.
So What Can You Try Today?
✅Support the arm: Use pillows, lap trays, or arm rests to avoid hanging or pulling.
✅ Sleep smart: Avoid sleeping on your affected shoulder. Try placing a pillow under your arm to keep it supported
✅Lean gently into your elbow to get that safe weight-bearing.
✅Use your good hand to help move your affected arm, especially when lying down — it reduces bad movement habits.
✅Add gentle external rotation — palm facing out, not in.
✅ Talk to a rehab therapist (especially ortho or neuro PTs) about scapular mobilization — getting the shoulder blade moving correctly can unlock a lot of pain relief.
Reflect On This:
-
What’s the real reason my shoulder might be hurting?
-
Am I chasing pain or addressing the cause?
-
Have I given my body the support it needs to move well?
Wrapping It Up
I know shoulder pain after stroke gets brushed off all the time.
But there’s always a reason behind it.
And when you understand what your body is trying to tell you, you can finally start making progress.
Check out this playlist on every single root cause of post-stroke shoulder pain.
Pain is not the end of your story.
It’s just the part that says:
“Look closer.”
And when you do — healing gets a whole lot more possible.
Articles you may be interested in
Walking Exercises for Stroke Patients
Many people inquire about the "best exercises" for stroke patients to improve walking. I like to use the term "Drills" when referring to "stroke exercises". Why? Because "Drills" are what I think of when I think of repetitive movement. Case and point, drills are...
Hemineglect after a stroke: When half the world is missing
hemineglect is a condition where someone loses the ability to attend to, sense, and/or perceive information on one side. This condition is also referred to as unilateral neglect, spatial neglect, and/or hemispatial neglect. Several neurologic condition can cause this...
Post Stroke Pain: Diagnosis and Treatment
Pain is a common symptom after a stroke. Unfortunately, pain can be a significant barrier to regaining function. In some cases, there is an identifiable cause related to a movement or a structural problem. The rehab team can identify this, prescribe the...
Tips for effective physical therapy at home after a stroke
An effective physical therapy program at home after a stroke is the most critical component for a successful recovery. I dare say MORE important than face to face time with your therapists. As someone who earns a living by treating patients (in person), this is a...
Caregiver Training: Helping someone stand
Standing is one of the most critical skills to relearn after any type of neurologic injury. Standing helps with digestion, bone health, and joint health. It can also reduce spasticity, and facilitate motor recovery. The caregiver role is almost more important than...
Walking After Stroke (Early Stage)
Walking after a stroke is important to a ton of stroke survivors. A stroke causes hemiplegia (weakness on one side of the body which can make standing and walking difficult. With this in mind, I get a ton of questions from stroke survivors and their...
Brunnstrom Stages of Motor Recovery
The Brunnstrom stages of stroke recovery is one proposed model of how someone with hemiplegia will recover movement. It was developed by a physical therapist in the 1960s and proposes that this sequence of recovery falls into six loosely defined stages. The main...
Gym Ball Exercise Routine for Better Balance
A Gym ball exercise routine is a great way to improve your balance. If provided with the correct exercises, they can challenge almost every "problem area" for a stroke survivor. The main areas that are problematic after a stroke are steadiness, symmetry, and dynamic...
Spastic ankle guide to stretching
Stretching a spastic ankle is critical to improve standing and walking. However, stretching a spastic ankle can also be extremely challenging. Add to that, NOT stretching a spastic ankle and you are at risk for making it worse. Ugh..... All that being said, never...
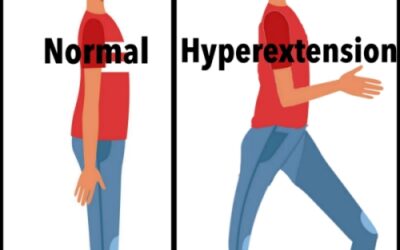
Knee Hyperextension after a Stroke: Causes and Treatment
What is Knee Hyperextension after a Stroke? Knee hyperextension is a common problem after a stroke. Knee hyperextension is when the knee goes beyond a straight position. Yeah, not exactly natural looking or feeling. ? Knee hyperextension (recurvatum) usually happens...