Why Does My Shoulder Hurt After a Stroke?
Understanding the 6 Most Common Causes and What You Can Actually Do About Them

Let’s be real — if you’re recovering from a stroke and your shoulder still hurts, it can feel really defeating.
Especially if you’ve been doing “all the things” — exercises, therapy, maybe even injections — and nothing seems to help.
Here’s what I want you to know:
Pain isn’t the problem.
It’s a signal that something needs attention.
So today, I want to walk you through the real reasons your shoulder might still be hurting — and what you can do about it.
Why Medications Alone Don’t Work
Medications may dull the pain, but they won’t fix the cause. Worse, they can delay real treatment. Pain is your body’s signal that something’s off. Covering it up without investigating why it’s there just prolongs the problem.
What’s Actually Causing the Pain?
There are several things that can lead to shoulder pain after a stroke.
But today I want to zoom in on just a few things that I think a lot of you might be missing.
1. Shoulder Subluxation
This is super common after a stroke.
Subluxation basically means your arm bone isn’t sitting fully in the shoulder socket.
And that little “drop” can stretch out soft tissue and cause a ton of pain.
But here’s the tricky part — sometimes you won’t even feel the subluxation.
You’ll just feel pain and not know why.
Try this:
-
- Gentle weight-bearing.

That doesn’t mean a full push-up. It might just mean sitting and leaning gently into your elbow.
That subtle pressure helps push the arm bone back into the socket.
It also gives the shoulder the feedback it needs to relearn how to stay stable.
Start small. Even a few minutes a day makes a difference.
- Positioning
Supporting the arm — especially when sitting or standing — is key.
2. Shoulder Impingement
This one happens when structures inside your shoulder (like tendons or bursa) get pinched —
usually because the shoulder blade or arm bone is in the wrong position.
And here’s the kicker:
You can accidentally cause this if your posture is off, or you’re trying to push through movement without the shoulder blade being supported.
What helps:
Doing movements lying down.
It’s also less effort, so your body stays more relaxed. That helps reduce compensation and spasticity, too.
Avoid pulleys or raising your arm too high until you’ve improved how your shoulder blade moves.
3. Adhesive Capsulitis (Frozen Shoulder)

This is when the joint capsule around your shoulder tightens up — like shrink-wrap. It severely limits how far your shoulder can move and can cause a deep, nagging pain, especially with lifting.
It often sneaks in when the shoulder isn’t being moved enough in all directions, especially external rotation (that out-to-the-side movement you need for things like reaching back into a jacket sleeve).
What helps:
Consistent, gentle stretching — especially external rotation.
This is where I recommend the Shoulder Flex tool. I started using it with clients because it allows a safe, supported stretch into that sticky range. Eventually, I started carrying it in our store because it’s just that helpful.

4. Spasticity
When your brain thinks it needs to work hard, it tightens everything.
You try to lift your arm, and suddenly your shoulder hikes up, your elbow locks, your wrist curls. That’s spasticity.
But here’s the twist:
Sometimes it’s not spasticity.
It’s just your brain trying to help… in all the wrong ways.
What helps:
Active assisted movement.
Especially lying down.
Use your good hand to help the weak arm.
You’ll be less likely to overcompensate. Less spasticity. Better alignment.
And the more your shoulder moves the right way, the more your brain relearns what “normal” feels like.
5. CRPS (Complex Regional Pain Syndrome)
This one’s tough. If you have CRPS, you probably know it’s not just shoulder pain — it’s pain that doesn’t make sense.
Your skin might be sensitive. Light touch might hurt. It feels like your body is on high alert.
What helps:
Progressive exposure to movement.
That means starting with what you can tolerate. Maybe you just rest your hand on a pillow. Maybe you just think about moving it.
There’s no rushing this. But you can retrain the brain to feel safe again.
6. Bursitis or Tendonitis
What it is:
Overuse or poor movement patterns can irritate the shoulder’s tendons or bursae (the cushions between joints).
What it feels like:
Pain that shifts or worsens with activity. It’s often mistaken for other shoulder problems.
What helps:
Reduce inflammation first — rest, ice, gentle motion. Long term, improve how the shoulder moves to avoid flare-ups.
So What Can You Try Today?
✅Support the arm: Use pillows, lap trays, or arm rests to avoid hanging or pulling.
✅ Sleep smart: Avoid sleeping on your affected shoulder. Try placing a pillow under your arm to keep it supported
✅Lean gently into your elbow to get that safe weight-bearing.
✅Use your good hand to help move your affected arm, especially when lying down — it reduces bad movement habits.
✅Add gentle external rotation — palm facing out, not in.
✅ Talk to a rehab therapist (especially ortho or neuro PTs) about scapular mobilization — getting the shoulder blade moving correctly can unlock a lot of pain relief.
Reflect On This:
-
What’s the real reason my shoulder might be hurting?
-
Am I chasing pain or addressing the cause?
-
Have I given my body the support it needs to move well?
Wrapping It Up
I know shoulder pain after stroke gets brushed off all the time.
But there’s always a reason behind it.
And when you understand what your body is trying to tell you, you can finally start making progress.
Check out this playlist on every single root cause of post-stroke shoulder pain.
Pain is not the end of your story.
It’s just the part that says:
“Look closer.”
And when you do — healing gets a whole lot more possible.
Articles you may be interested in
How to Fix a Trendelenburg Gait
Why Your Hip Drops When You Walk : How to Regain Stability https://youtu.be/37akItHE9mcHave you ever noticed that one side of your hip drops lower when you walk? Maybe someone pointed it out, or you feel off-balance or unsteady when taking steps. This could be a sign...
Correct Knee Hyperextension after a Neurologic Injury
Struggling with Knee Hyperextension? Here's How to Fix It! Does your knee snap backward when you walk? Do your steps feel jerky, unsteady, or inefficient? If so, you might be dealing with knee hyperextension, a common issue after a stroke, brain injury, or...
How to Fix a Vaulting Gait
How to Stop Vaulting and Walk More Naturally After a Stroke If you’ve ever noticed yourself pushing up on your stronger leg to swing your weaker leg forward while walking, you may be experiencing vaulting. The good news? Vaulting can be unlearned with the right...
How to Fix Circumduction and Walk Better
Why Your Leg Swings Out: Causes and Exercises to Improve Gait https://youtu.be/mXI9oaJ6uHkCircumduction is a common issue after a stroke, where your leg swings out to the side instead of moving straight forward as you walk. This abnormal gait pattern can be...
Discover 15 Principles to Rewiring Your Brain Faster
Discover 15 Principles to Rewiring your Brain Faster Transform Your Mindset and Achieve Rapid Results https://youtu.be/rfSCk_qJe64 Neuroplasticity: Your Brain’s Superpower After a stroke, the brain can suffer damage, but it’s far from the end. But here’s the good...
Eye Exercises for Stroke Survivors: Regaining Vision and Function
Visual impairment is a very common consequence in stroke survivors—almost 50% of stroke survivors become visually impaired. This is primarily because the brain's visual pathways are blocked or damaged when a person experiences a stroke. As a result, patients often...
Pontine Stroke: Everything you need to know
https://youtu.be/bynfAyJNM_8 A Pontine Stroke is commonly referred to as a pontine CVA or pontine cerebrovascular accident. It is an ischemic stroke that affects a region in the brain stem known as the pons. Not sure why this is important? The pons communicates...
Understanding Learned Non-Use
https://youtu.be/iLo0j4aC44I Do you feel like you have plateaued? What I mean is, has your arm and leg movement recovery slowed to a crawl? Or maybe progress has stopped altogether? The common belief is that someone loses the ability to move because that part...
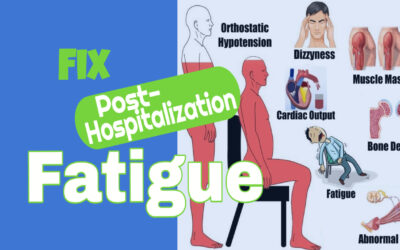
Post Hospitalization Fatigue: What causes it and how to do fix it?
Do you ever feel so tired, you don't even want to get out of bed? If so, you wouldn't be alone. There is a really good reason for this. Fatigue is an extremely common problem after a hospitalization. And sometimes, it has nothing to do with the reason you were...
Discharged from therapy. What now?
So, you have been discharged from therapy. So, what now? For some, this is a positive step in the rehab process. Some will understand right away that this is progress. On the other hand, for others it can bring up all kinds of negative emotions. "Is my therapist mad...