8 Common Stretching Mistakes in Stroke Recovery
Why Your Stretching Might Be Making Spasticity Worse
If you’re dealing with spasticity after a neurologic injury, stretching might not be as straightforward as it seems. In fact, doing it the wrong way can increase resistance, worsen symptoms, and set your progress back.
Spasticity vs. Tightness: Know the Difference
One of the most common misconceptions is treating spasticity like muscle tightness. Spasticity is an involuntary muscle contraction due to a loss of connection with parts of the brain that help to inhibit overactive movements. While a tight muscle simply needs lengthening, a spastic muscle resists lengthening and often contracts more with speed or stimulation. That’s why standard stretching techniques don’t always work.
The 8 Stretching Mistakes to Avoid
- Prolonged Holds Without Movement
Long static holds may help tight muscles but not spastic ones. Instead, incorporate slow, rhythmic movements to help desensitize the muscle. - Stretching Too Fast
Spasticity is velocity-dependent, which means the faster you stretch, the worse it gets. Go slow, always. - Only Stretching Once a Day
Even 30 minutes of stretching isn’t enough if the muscle contracts involuntarily the rest of the day. Wearing a properly fitted splint can help maintain gains. Most off-the-shelf splints aren’t strong enough to resist spastic contractions. Use one designed for neurologic conditions, or you can order our Rehab HQ hand brace. - Stretching in the Wrong Position
Stretching in unsupported or upright positions may trigger more resistance. Support the arm or lie down to reduce stimulation. - High-Stimulation Environments
Noisy, bright, or stressful environments increase spasticity. Do your stretching in a calm, quiet, low-stimulation space. - Lack of Active Engagement
Combine passive stretches with active-assisted or antagonist muscle activation to promote balance and relaxation. - Skipping Weight-Bearing Stretches
Weight-bearing (e.g., standing calf stretches or resting your forearm on a table) can reduce spasticity more effectively than sitting. - Engage Your Brain
Don’t mentally check out. Engaging your brain during stretching by mentally focusing on relaxing the muscle can help with inhibition and improve results over time.
Final Thoughts
Stretching spastic muscles requires more than just time and effort, it demands the right strategy. By avoiding these common mistakes and using techniques tailored for spasticity, you can reduce resistance, improve muscle control, and make your stretching routine more effective.
Consistency, proper positioning, and staying mentally engaged are key. With the right tools and guidance, you can take meaningful steps toward better mobility and recovery.
Tools to Supercharge Your Recovery
Want a comprehensive rehab plan without bouncing between therapists or feeling lost?
Our Gold Membership Program includes:
- Ad free videos and handouts
-
Full access to 350+ home rehab exercise videos
-
Monthly Q&A sessions and webinars
-
A private discussion board I check daily
👉 Learn more at Rehab HQ
📞 Or schedule a discovery call to find out if it’s right for you.
🖐 Rehab HQ Hand Brace Ordering Form
🟦 ShoulderFlex (Blue Shoulder Stretching Tool)
Articles you may be interested in
3 Big Balance Mistakes After Stroke—and How to Fix Them
Have you ever felt like your balance is fine at home… but the moment you step outside, it’s a totally different story? You’re not alone—and there’s a good reason for that. I talk to a lot of people who say, “I feel pretty confident walking around my house, but the...
Post Stroke “help” isn’t helpful: A Lesson from the Butterfly
“We delight in the beauty of the butterfly, but rarely admit the changes it has gone through to achieve that beauty.” — Maya Angelou “If only I had more help”… More therapy. More equipment. More family support. “Then things would be different. I would be different....
Neuroplasticity and Recovery: How Life’s Loops Shape Growth and Transformation
"The adventure of life is to learn. The purpose of life is to grow. The nature of life is to change." — Unknown “Why run that far when you have a perfectly reliable car?” Back in my marathon days, this rhetorical question was something I heard more times than I can...
Stroke Recovery for the Brain: Boost Memory, Focus, and Thinking Skills
Stroke Recovery for the Brain: Boost Memory, Focus, and Thinking Skills We often talk about walking again. Moving your arm again. Lifting your leg. And yes—those goals are important. But here’s what we don’t talk about enough: That moment you walk into a room and...
The Secret to Stroke Recovery Success
"The secret to winning is learning how to lose. That is, learning to bounce back from failure and disappointment—undeterred—and continuing to steadily march toward your potential. Your response to failure determines your capacity for success." -James Clear, author of...
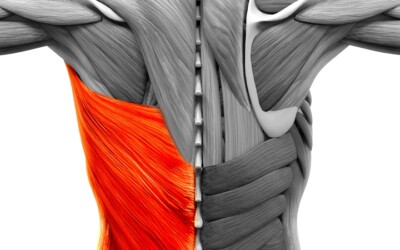
The Hidden Culprit: How the Latissimus Dorsi Limits Shoulder Recovery After Stroke
The Hidden Culprit: How the Latissimus Dorsi Limits Shoulder Recovery after Stroke It’s the silent barrier most people never think about. When we talk about restoring arm movement after a stroke, most of the focus is on the obvious: the shoulder joint, the triceps,...
How to Fix Knee Buckling Post Stroke
Why Your Knee Buckles—and How to Regain Control Say Goodbye to Knee Giving Way and Hello to Confident Walking https://youtu.be/wNZxiTXTz7QWhat Is Knee Buckling? Knee buckling refers to a sudden, unexpected loss of stability in the knee joint, often described as the...
Understanding and Fixing Leg Cramps Post Stroke
Clonus Explained: What It Is, Why It Happens, and What You Can Do About It Stop Letting Leg Cramps Slow Your Recovery https://youtu.be/fGNGXoMSvT4 Can Clonus Affect the Way You Walk? Absolutely—Here’s What You Need to Know Have you ever felt your foot suddenly...
Why Your Hand Still Won’t Open After Stroke | 3 Mistakes to Fix
Why Forcing It Doesn't Work How to Stop Reinforcing the Wrong Patterns and Start Rewiring Your Brain for Real Recovery https://youtu.be/fDIgGLM8Kj0If you’ve had a stroke (or other neurologic injury), and your hand feels like it’s stuck in a fist or your arm just hangs...
Understanding Abnormal Synergy Patterns After Stroke: The Missing Puzzle Piece in Recovery
Understanding Abnormal Synergy Patterns After Stroke: The Missing Puzzle Piece in Recovery Stroke recovery is rarely straightforward.You might work on strength, balance, and mobility—yet your movements still feel awkward, stiff, or “robotic.” Why?One of the most...