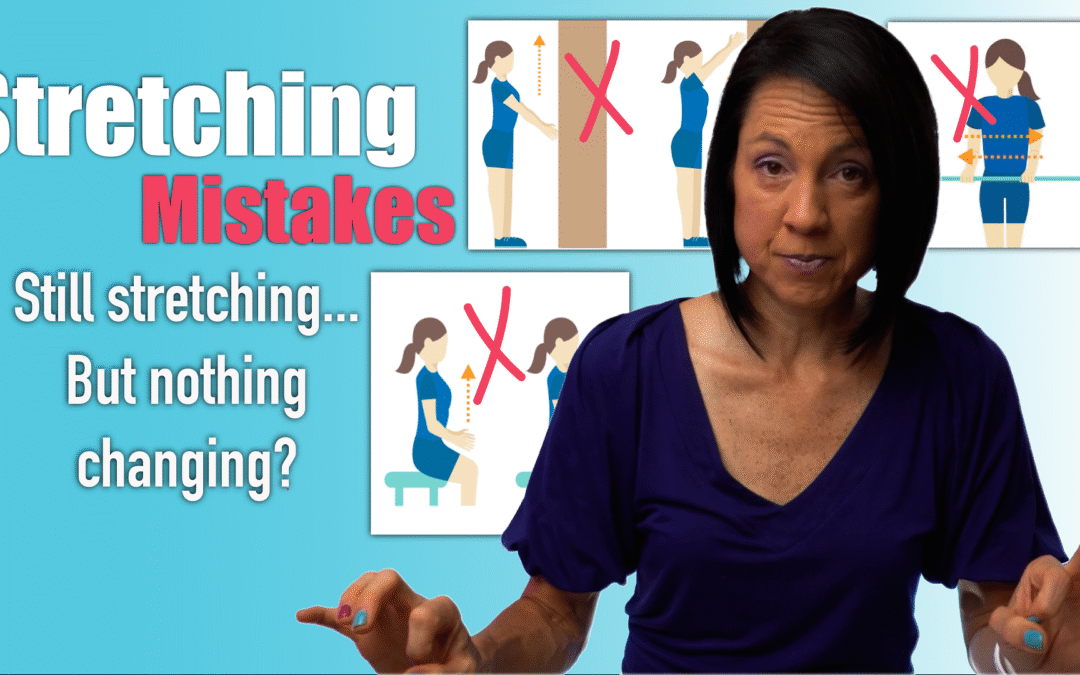
8 Common Stretching Mistakes in Stroke Recovery
Why Your Stretching Might Be Making Spasticity Worse
If you’re dealing with spasticity after a neurologic injury, stretching might not be as straightforward as it seems. In fact, doing it the wrong way can increase resistance, worsen symptoms, and set your progress back.
Spasticity vs. Tightness: Know the Difference
One of the most common misconceptions is treating spasticity like muscle tightness. Spasticity is an involuntary muscle contraction due to a loss of connection with parts of the brain that help to inhibit overactive movements. While a tight muscle simply needs lengthening, a spastic muscle resists lengthening and often contracts more with speed or stimulation. That’s why standard stretching techniques don’t always work.
The 8 Stretching Mistakes to Avoid
- Prolonged Holds Without Movement
Long static holds may help tight muscles but not spastic ones. Instead, incorporate slow, rhythmic movements to help desensitize the muscle. - Stretching Too Fast
Spasticity is velocity-dependent, which means the faster you stretch, the worse it gets. Go slow, always. - Only Stretching Once a Day
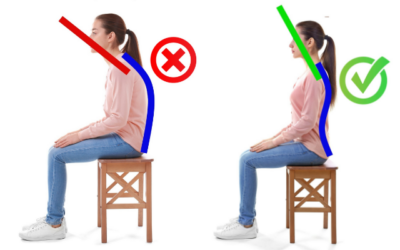
Even 30 minutes of stretching isn’t enough if the muscle contracts involuntarily the rest of the day. Wearing a properly fitted splint can help maintain gains. Most off-the-shelf splints aren’t strong enough to resist spastic contractions. Use one designed for neurologic conditions, or you can order our Rehab HQ hand brace. - Stretching in the Wrong Position
Stretching in unsupported or upright positions may trigger more resistance. Support the arm or lie down to reduce stimulation. - High-Stimulation Environments
Noisy, bright, or stressful environments increase spasticity. Do your stretching in a calm, quiet, low-stimulation space. - Lack of Active Engagement
Combine passive stretches with active-assisted or antagonist muscle activation to promote balance and relaxation. - Skipping Weight-Bearing Stretches
Weight-bearing (e.g., standing calf stretches or resting your forearm on a table) can reduce spasticity more effectively than sitting. - Engage Your Brain
Don’t mentally check out. Engaging your brain during stretching by mentally focusing on relaxing the muscle can help with inhibition and improve results over time.
Final Thoughts
Stretching spastic muscles requires more than just time and effort, it demands the right strategy. By avoiding these common mistakes and using techniques tailored for spasticity, you can reduce resistance, improve muscle control, and make your stretching routine more effective.
Consistency, proper positioning, and staying mentally engaged are key. With the right tools and guidance, you can take meaningful steps toward better mobility and recovery.
Tools to Supercharge Your Recovery
Want a comprehensive rehab plan without bouncing between therapists or feeling lost?
Our Gold Membership Program includes:
- Ad free videos and handouts
-
Full access to 350+ home rehab exercise videos
-
Monthly Q&A sessions and webinars
-
A private discussion board I check daily
👉 Learn more at Rehab HQ
📞 Or schedule a discovery call to find out if it’s right for you.
🖐 Rehab HQ Hand Brace Ordering Form
🟦 ShoulderFlex (Blue Shoulder Stretching Tool)
Articles you may be interested in
Neuro Rehab is 90% mental, 10% physical
What should you expect to achieve in neurologic rehabilitation? My answer might confuse you, frustrate you, and hopefully challenge you to think differently. The most critical component of a successful outcome (in neurologic rehabilitation) is NOT based on the extent...
Hemiplegia: Fix a side bent trunk
Hemiplegia (weakness on one side of the body) can cause an unnatural "side bent" posture. This is sometimes also referred to as lateral trunk flexion. What is a "side bent" posture (lateral trunk flexion) with hemiplegia? A side bent posture is a “structural problem”...
Physical therapists are not as important as they think
I am not as important as I think I am. More broadly, physical therapists are NOT as important (to a rehab plan) as they may think. No, seriously. Ok, maybe half seriously. 2020 has been "unprecedented" (I couldn’t resist 🙃). I did what I thought I would never do....
Balance Training for Ataxia
Balance training is a critical component for anyone with ataxia. This is due to the fact that ataxia negatively impacts the balance system and is one of the leading causes of disability. Ataxia is caused by damage to the cerebellum. The cerebellum plays a MAJOR role...
5 Problems that Lead to Circumduction
Circumduction is a “walking problem” that is characterized by the leg swinging out to the side. This is typically a compensatory strategy to prevent someone from catching the foot on the ground. Before we dive into what might be causing you to swing the leg around the...
Managing Fatigue with a Neurologic Condition
Fatigue is a major problem with a variety of neurologic conditions. Feeling fatigued can be a HUGE barrier in your physical recovery and it can also dramatically impact your overall quality of life.That being said, managing fatigue might be the single most important...
Movement Retraining when dealing with Spasticity
Spasticity is an involuntary muscle contraction due to damage to the brain or spinal cord. This can cause muscle stiffness and pain. Additionally, involuntary muscle contractions cause the body to move in ways that feel out of one’s control. This is turn can create...
Complete Guide to Buying a Wheelchair Cushion
Wheelchairs are an extremely valuable piece of equipment during the neurologic recovery process. They provide a means of getting around when walking is not safe and/or is not possible. However, they also come with the risk of developing pressure ulcers. Pressure...
Most Neglected Post Stroke Shoulder Exercise
Post stroke shoulder retraining often includes moving the arm bone. Unfortunately, many movement retraining programs fail to address the shoulder blade (flat bone on the back of the shoulder and the thoracic spine. Moving the humerus requires proper movement of the...
Relearn to walk: Progression (with videos)
Are you super eager to relearn to walk? Walking is a HUGE goal for anyone who has lost that ability. Walking means different things to different people. And quite honestly, has far less meaning until you have lost this fundamental skill. All that being said, it is...