How Can You Tell If It’s Spasticity or Weakness After Stroke?
If you’ve had a stroke, you’ve probably heard a few of these words tossed around: spasticity, weakness, stiffness, foot drop. They might all sound similar, but they each tell a different story about what’s going on in your muscles and your brain.
Knowing the difference isn’t just medical jargon, it’s the key to picking the right exercises, making faster progress, and feeling more in control of your recovery.
1. Spasticity: When the Muscle Contracts Without Your Permission
Spasticity is an involuntary muscle contraction caused by damage to the brain or spinal cord.
It’s what we call velocity-dependent, meaning the faster you try to move a muscle, the stronger the resistance you feel.
So what does that feel like?
Maybe your arm suddenly tightens when you try to move it fast, or your ankle resists when you try to lift your foot. Sometimes it feels fine, and other times, it stiffens up for no reason.
Inside your body, this happens because there’s too much voltage. Too many signals telling your muscles to contract, and not enough signals telling them to relax.
Terms in Physical Therapy to Describe Movement
Understanding the language your therapist uses can help you better recognize what’s happening in your body. Here are a few key terms:
-
Clonus: a set of involuntary and rhythmic muscular contractions and relaxations. It’s often a sign of certain neurologic conditions involving the brain or spinal cord, particularly those that affect motor pathways. It can cause the foot to point downward repeatedly or “bounce.”
-
Toes curling: when the toes involuntarily bend or point downward due to increased muscle tone.
-
Ballistic movements / jerky movements: sudden, uncontrolled muscle contractions where the muscle either fires fully or not at all, no smooth in-between control.
Common signs of spasticity include:
- Scissoring or leg swinging when walking
A spastic muscle isn’t a strong muscle. It’s overactive and uncoordinated, which can make movement feel out of your control.
How to Help Spastic Muscles Relax
Managing spasticity is all about turning the voltage down and calming the nervous system. Here’s how you can help that process:
- Low-stimulation environment: Try doing your therapy or stretching somewhere quiet and calm. Too much stimulation can make spasticity worse.
- Inhibition strategies: Focus on relaxation exercises like deep breathing, slow movements, and gentle holds.
- Move and stretch slowly: Fast stretches increase resistance; slow ones promote relaxation.
- Weight-bearing: Standing stretches or gentle pressure through the affected limb help calm muscle overactivity.
- Sensory input: Tools like a vibration plate or a massage gun can help reduce spasticity.
Important: If you’re using an AFO (ankle-foot orthosis) talk with your medical provider or therapist to make sure it fits your needs safely.
2. Weakness (Hemiparesis): When the Brain Loses Its Connection
Weakness after a stroke or what therapists call hemiparesis, feels more like a floppy limb.
Your arm or leg may just hang there, or your foot might dangle and drag when you walk.
This isn’t just a muscle problem. It’s a neural network issue. Your brain has lost some of the automatic pathways that control movement.
The good news? Those pathways can be rebuilt through repetition.
Every time you move that limb with focus and intention, you’re helping your brain lay down new “tracks.”
Rebuilding movement takes patience, but it’s absolutely possible. Even slow progress means your brain is reconnecting.
3. Stiffness: When Muscles Shorten Over Time
Stiffness is different from spasticity. It’s not caused by the brain sending too much signal, it’s a muscle issue that develops from staying in one position for too long.
When a muscle isn’t stretched enough, it adaptively shortens. You might notice your arm doesn’t straighten all the way or your ankle feels tight.
To improve stiffness:
- Use prolonged stretching. Gentle, consistent holds that encourage the muscle to lengthen.
- Consider splinting or braces to support proper positioning.
- For the ankle, an AFO with a plantar flexion stop can prevent contractures and keep the foot from pointing down.
- If you already have a contracture, your therapist may use a wedge under the AFO to safely support your foot position. Always check with your clinician before making adjustments.
Putting It All Together
Let’s recap:
- Spasticity – This happens when your muscles are overactive, sending too much “voltage.” The focus here is on relaxation: slow, controlled movements and calming your nervous system can help manage it.
- Weakness (Hemiparesis) – This occurs when neural connections are lost, making movement difficult. Retraining the brain with repetition and focused practice is key to rebuilding strength and coordination.
- Stiffness – Muscles that have shortened due to immobility can feel tight all the time. Gentle, prolonged stretching along with proper support, like splints or braces, can help restore mobility.
You might have one, or you might have a mix of all three, and that’s okay. The important thing is knowing why something feels the way it does so you can choose the best exercises for your body.
If you’re still unsure whether what you’re feeling is spasticity, weakness, or stiffness, don’t guess alone. Talk with your physical or occupational therapist. Understanding what’s going on in your body is the first step to making real, lasting progress.
And remember, recovery is not about being perfect. It’s about being consistent, curious, and patient with yourself. Every stretch, every repetition, every effort you make brings your brain and body closer to working together again.
Take Control of Your Rehab
Understanding these differences is the first step toward effective recovery. If you want guided support, personalized exercises, and a community to keep you motivated, check out our Membership Plans here. Get access to our full exercise library, monthly Q&As, and tools to help you move better and feel stronger every day.
Supplemental Videos
Articles you may be interested in
Hemiplegia: Fix a side bent trunk
Hemiplegia (weakness on one side of the body) can cause an unnatural "side bent" posture. This is sometimes also referred to as lateral trunk flexion. What is a "side bent" posture (lateral trunk flexion) with hemiplegia? A side bent posture is a “structural problem”...
Physical therapists are not as important as they think
I am not as important as I think I am. More broadly, physical therapists are NOT as important (to a rehab plan) as they may think. No, seriously. Ok, maybe half seriously. 2020 has been "unprecedented" (I couldn’t resist 🙃). I did what I thought I would never do....
Balance Training for Ataxia
Balance training is a critical component for anyone with ataxia. This is due to the fact that ataxia negatively impacts the balance system and is one of the leading causes of disability. Ataxia is caused by damage to the cerebellum. The cerebellum plays a MAJOR role...
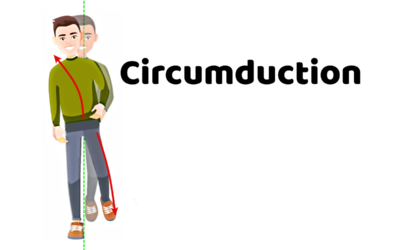
5 Problems that Lead to Circumduction
Circumduction is a “walking problem” that is characterized by the leg swinging out to the side. This is typically a compensatory strategy to prevent someone from catching the foot on the ground. Before we dive into what might be causing you to swing the leg around the...
Managing Fatigue with a Neurologic Condition
Fatigue is a major problem with a variety of neurologic conditions. Feeling fatigued can be a HUGE barrier in your physical recovery and it can also dramatically impact your overall quality of life.That being said, managing fatigue might be the single most important...
Movement Retraining when dealing with Spasticity
Spasticity is an involuntary muscle contraction due to damage to the brain or spinal cord. This can cause muscle stiffness and pain. Additionally, involuntary muscle contractions cause the body to move in ways that feel out of one’s control. This is turn can create...
Complete Guide to Buying a Wheelchair Cushion
Wheelchairs are an extremely valuable piece of equipment during the neurologic recovery process. They provide a means of getting around when walking is not safe and/or is not possible. However, they also come with the risk of developing pressure ulcers. Pressure...
Most Neglected Post Stroke Shoulder Exercise
Post stroke shoulder retraining often includes moving the arm bone. Unfortunately, many movement retraining programs fail to address the shoulder blade (flat bone on the back of the shoulder and the thoracic spine. Moving the humerus requires proper movement of the...
Relearn to walk: Progression (with videos)
Are you super eager to relearn to walk? Walking is a HUGE goal for anyone who has lost that ability. Walking means different things to different people. And quite honestly, has far less meaning until you have lost this fundamental skill. All that being said, it is...
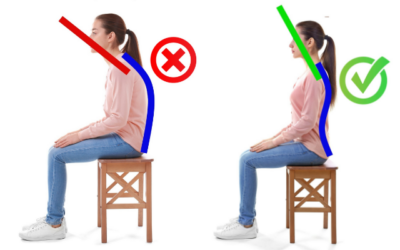
Product Spotlight: This tool improves trunk alignment
Better posture means better arm rehabilitation. Period. Said another way, proper trunk alignment is essential for efficient arm movement. However, in most cases, hemiparesis (weakness on one side of the body), paraparesis (weakness on the lower half of the body), and...