Why Your Knee Buckles—and How to Regain Control
Say Goodbye to Knee Giving Way and Hello to Confident Walking
What Is Knee Buckling? 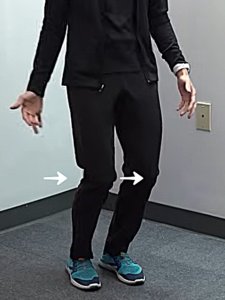
Knee buckling refers to a sudden, unexpected loss of stability in the knee joint, often described as the knee “giving way.”
It can happen while standing, walking, or going up and down stairs. This issue may stem from muscle weakness, poor coordination, or involuntary muscle patterns following a neurological injury or condition.
What Causes Knee Buckling?
1. Weakness – Often in the quadriceps (the muscles that straighten the knee) or the plantarflexors (calf muscles that point the foot down). This is common in peripheral neuropathies like diabetes.
2. Lack of Eccentric Control – Eccentric control is the ability of muscles (especially the quads) to lengthen while contracting. For example, this is needed when going down stairs.
3. Inability to Dissociate – After a stroke, the brain may struggle to make the legs perform separate movements. This may cause buckling even in the stronger leg.
4. Abnormal Synergy Patterns – Like the flexor synergy pattern, where involuntary movements cause the leg to bend unexpectedly, similar to the reflex babies use.
Flexor Withdrawal – An automatic reaction where the leg pulls away in response to a sensation on the sole of the foot.
5. Spasticity – Involuntary muscle contractions that occur due to brain or spinal cord damage. Spasticity is different from dystonia and can make coordinated movement difficult.
How Bracing Can Help
1. Floor Reaction AFO (Ankle-Foot Orthosis)
This brace helps by pushing your shin bone backward, giving your knee more support when you stand or walk.
✅ Best for:
- Knee buckling from weak quadriceps
-
Flexor synergy patterns (common after a stroke or brain injury)
🦶 Why it works:
It supports your knee by adjusting your ankle position—addressing the problem from the ground up.
2. Knee Immobilizer (Training Tool) 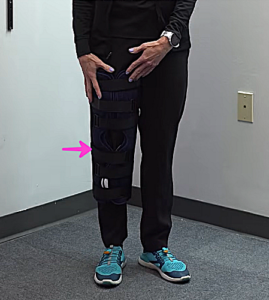
This brace keeps your knee locked straight to help retrain your leg muscles.
✅ Best used for:
-
Weakness in the quads
-
Early stages of spasticity
-
Difficulty making both legs move differently (poor dissociation)
⚠️ Important:
This is not for regular walking. It’s a short-term training tool to build better control during early rehab.
Exercises to Improve Knee Stability
I. Strengthening the Calf Muscles
- Stand using a chair or anything stable for support.
- Do single-leg toe raises.
Modification 1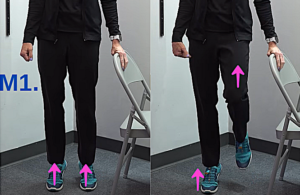
- Go up with both feet
- Lift one foot
- Lower slowly.
Modification 2
- Step back from the chair
- Lean forward
- Raise heels without bending the knees.
II. Sit to Stand (STS) for Quad Strength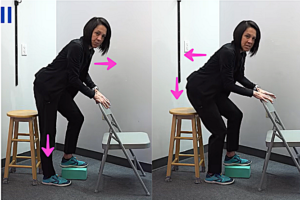
- Sit on a stool holding onto a chair for stability.
- Place your non-working leg on a yoga block.
- Shift weight to the working leg.
- Lean forward and push up (concentric).
- Lower down slowly (eccentric).
Progression: Begin on a high stool and progress to lower surfaces.
III. Step Training with PVC Frame
A. Step Up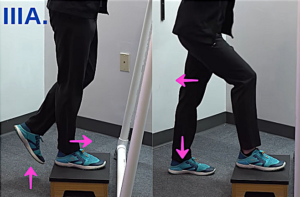
- Stand in front of a wide step or low platform.
- Step up using your stronger leg. This is the “push” part where your muscles are doing most of the work. (concentric)
- Step back down slowly and with control. (eccentric)
B. Step Down Over the PVC Frame
- Step up like before.
- Now, carefully step forward and down over the PVC frame. (concentric)
- This part focuses on controlled movement as your leg muscles slowly lower your body. (eccentric)
 IV. Dissociation Training
IV. Dissociation Training
- Sit on a high stool with your weaker leg bent over a chair in front of you.
- Place your hands on the chair for support and balance.
- Try to perform a sit-to-stand, keeping one leg bent and the other straight the entire time.
➡️ The key is to make sure your leg positions are in the extremes—one bent, one straight—to truly work on dissociation.
Progression: Switch leg positions and repeat the exercise with the opposite setup.
Too difficult?
-
-
Start in standing with a knee immobilizer on the weaker leg.
-
Conclusion
Struggling with knee buckling can feel frustrating and even a little scary—but it doesn’t have to stay that way. When you understand why it’s happening, whether from weakness, nerve issues, or changes after a stroke, you can start building a path forward. The right combination of braces, targeted exercises, and support from your rehab team can make a real difference.
Take the first step toward steadier, more confident walking—your recovery is worth it.
Articles you may be interested in
Best Foods for Brain Healing and Mental Clarity
Brain Recovery Nutrition How Diet Fuels Healing and Focus https://youtu.be/P5UJMJJRVdw When it comes to stroke recovery, exercise and rehab often take the spotlight. But what if the foods you eat and the nutrients inside them could also play a powerful role in healing...
Is Your Neuro Rehab Helping Your Recovery, or Making Things Worse?
The Real Impact of Neuro Rehab on Recovery https://youtu.be/YDgQc4p_atE Recovering after a stroke often involves long hours of rehabilitation. Neuro rehab programs are designed to retrain the brain and body, helping survivors regain independence. Understanding...
How Short Bursts of Exercise Boost Brain Healing
HIIT for Stroke Recovery Boost brain rewiring, improve movement, and speed recovery with short bursts of exercise. https://youtu.be/4SgXN2uRX8g If you’ve been on your stroke recovery journey for a while, you’ve probably heard the word neuroplasticity. Neuroplasticity...
Stretching Spastic Muscles: 8 Mistakes to Avoid
8 Common Stretching Mistakes in Stroke Recovery Why Your Stretching Might Be Making Spasticity Worse https://youtu.be/bBsM34HROYY If you’re dealing with spasticity after a neurologic injury, stretching might not be as straightforward as it seems. In fact, doing it the...
New Study: Vibration Plates Boost Balance After Stroke
It Just Vibrates… So Why Are Stroke Survivors Getting Better? The Truth Behind the Research https://youtu.be/GZgGsMjEgJQ When vibration plates first became popular, they reminded many of us of those old 1980s machines that promised to "shake" the fat away. Naturally,...
Walking “Tips” that Sabotage Post-Stroke Progress
Recovering from Stroke? Don’t Let These 7 Walking Mistakes Set You Back Better Walking Starts by Avoiding These Mistakes https://youtu.be/_nkjHLdOeLc Recovering your walking ability after a stroke is an incredible accomplishment. You’ve put in the work. Strengthening...
The Hidden Reason Your Walking Feels Off After Stroke Rehab
The Missing Link in Stroke Rehab: Why Strength Isn’t Enough How Plyometric Exercises Can Improve Your Post-Stroke Walking https://youtu.be/0xzcgTifCiM Recovering from a stroke is a journey that takes patience, effort, and persistence. Maybe you’ve been faithfully...
Struggling with Shoulder Pain After a Stroke? Here’s What Works
Why Does My Shoulder Hurt After a Stroke?Understanding the 6 Most Common Causes and What You Can Actually Do About Them Let’s be real — if you’re recovering from a stroke and your shoulder still hurts, it can feel really defeating. Especially if you’ve been doing “all...
Still Feeling Weak After Stroke? This Might Be Why
Doing the exercises… but still not getting stronger?You’re walking. You’re moving. Maybe even getting stronger.But everything still feels hard. Like walking across a room takes full concentration. Or standing up while talking feels like solving rocket science....
Stroke Recovery: Spasticity vs. Adaptive Shortening vs. Contracture
Stroke Recovery: Spasticity vs. Adaptive Shortening vs. Contracture Muscle tightness after stroke is common and can be the greatest barrier to restoring normal arm and leg movement. But not all tightness is the same. To treat it effectively, you need to understand...