Recovering from Stroke? Don’t Let These 7 Walking Mistakes Set You Back
Better Walking Starts by Avoiding These Mistakes
Recovering your walking ability after a stroke is an incredible accomplishment. You’ve put in the work. Strengthening exercises, therapy sessions, and daily practice. But what if your progress feels slower than expected? Or certain strategies just don’t feel quite right?
The truth is, some of the most common walking tips used in stroke rehab can unintentionally make things harder in the long run. Based on my professional experience working with stroke survivors, here are 7 mistakes that could be holding you back.
Mistake #1: Using a One-Handed Device on Your Strong Side
Example: A hemi-walker placed on your stronger arm right after a stroke.
It may seem logical to add stability to your strong side, but this often backfires, especially early in rehab. Devices like hemi-walkers have wide bases and offer so much support that they reinforce leaning and over-reliance on your strong side. This makes it harder to relearn balanced walking, and the habit is tough to unlearn.
What to try instead:
- Two caregivers for hand-held assistance, this encourages symmetry.
- A two-handed walker, possibly with your unaffected hand gently strapped to guide use of both sides.
- If compensations are already present, try placing the device in front of you and avoid keeping it off to the side.
- In the later stages of recovery, consider switching to a walking stick or trekking pole. These give support without encouraging one-sided leaning.
Mistake #2: Assuming Any AFO (Ankle-Foot Orthosis) Will Work
AFOs are often issued early in rehab, but not all are created equal. If your walking form or speed is off, the wrong AFO can make things worse, like stiffening your leg or limiting natural movement.
Real example: One client’s speed training hit a wall because her non-articulated AFO didn’t allow enough ankle flexibility. Once adjusted, her walking improved significantly.
What to try instead:
- Work closely with a physical therapist and orthotist to find an AFO tailored to your goals.
- If it’s not working, let them know. The best providers will try other solutions.
Mistake #3: Throwing Away Your AFO (Ankle Foot Orthosis) Too Soon
Sometimes a therapist says you “don’t need your AFO anymore.” While that may feel like progress, ditching it completely can lead to setbacks.
Here’s why: Spasticity never disappears fully. It’s always there in the background, and when compensations sneak back in, stiffness often follows.
What to try instead:
- Wean off your AFO gradually.
- Use it when walking in public or on long outings, but practice walking without it safely at home.
- Keep the AFO on hand. If spasticity returns, wear it for a week or two to reset.
Mistake #4: Focusing Too Much on Walking Quality Instead of Speed
This might sound counterintuitive, but speed and distance often matter more than form.
What to try instead:
- Prioritize speed and distance if you spend a lot of time in a wheelchair
- Work on a “normalized” walking form only if you’ve had no recent falls, and especially if it’s been years since your stroke.
Mistake #5: Focusing on “Heel-Toe” Cues
“Walk heel-toe” is common advice, but it might not be helping you.
Here’s the issue: Telling someone with spasticity to push off with their toe can actually increase toe pointing, delay foot clearance, and make foot drop worse.
What to try instead:
- Use the cue: “Heel, heel.” Eliminate “toe” from your vocabulary altogether.
- This gives your foot more time to clear the ground and helps prevent tripping.
Mistake #6: Only Strengthening Glutes
Many stroke survivors are told to “strengthen your glutes,” but stroke recovery is about retraining movement patterns, not just building muscle.
Why that matters: A stroke affects the brain’s ability to control movement, not the muscle’s ability to activate. For example, you might be able to squeeze your glute, but still struggle to stand on that leg without your hip dropping.
What to try instead:
- Focus on functional exercises like single-leg standing. Aim to hold your hip steady without dropping.
- Think movement, not just strength.
Mistake #7: “Don’t Look Down”
You’ve probably heard this one before, but it’s misleading. Looking down is normal and necessary for safe walking.
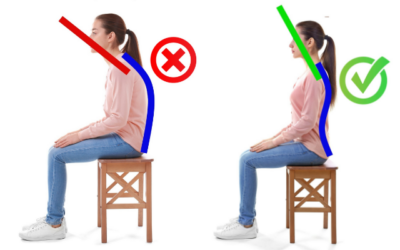
What’s actually dangerous is bending your head and shoulders forward to look at your feet.
What to try instead:
- Glance down with your eyes, not your head.
- Keep your neck upright and shoulders back.
- Look 6–10 feet ahead, but check the ground as needed, especially if you can’t fully feel your feet.
Final Thoughts
Stroke rehab is challenging, and there’s no one-size-fits-all solution. The key is understanding why something is being recommended, and making sure it truly supports your long-term goals.
If any of these tips resonated with you, try out the alternatives and see how they feel. Improving your walking isn’t just about strength or form. It’s about confidence, safety, and freedom.
Abnormal Muscle Synergies after a Stroke or Brain Injury
Abnormal muscle synergies are one of the most common "movement problems" after a stroke or brain injury. What is an abnormal muscle synergy? A flexor synergy is when the hip, knee, and ankle all flex at the same time (visualize drawing your knee into your chest). An...
Neuro Rehab is 90% mental, 10% physical
What should you expect to achieve in neurologic rehabilitation? My answer might confuse you, frustrate you, and hopefully challenge you to think differently. The most critical component of a successful outcome (in neurologic rehabilitation) is NOT based on the extent...
Hemiplegia: Fix a side bent trunk
Hemiplegia (weakness on one side of the body) can cause an unnatural "side bent" posture. This is sometimes also referred to as lateral trunk flexion. What is a "side bent" posture (lateral trunk flexion) with hemiplegia? A side bent posture is a “structural problem”...
Physical therapists are not as important as they think
I am not as important as I think I am. More broadly, physical therapists are NOT as important (to a rehab plan) as they may think. No, seriously. Ok, maybe half seriously. 2020 has been "unprecedented" (I couldn’t resist 🙃). I did what I thought I would never do....
Balance Training for Ataxia
Balance training is a critical component for anyone with ataxia. This is due to the fact that ataxia negatively impacts the balance system and is one of the leading causes of disability. Ataxia is caused by damage to the cerebellum. The cerebellum plays a MAJOR role...
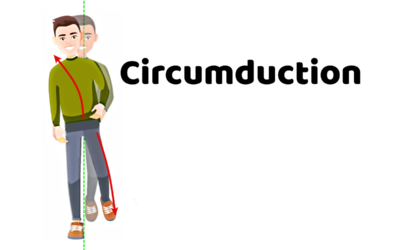
5 Problems that Lead to Circumduction
Circumduction is a “walking problem” that is characterized by the leg swinging out to the side. This is typically a compensatory strategy to prevent someone from catching the foot on the ground. Before we dive into what might be causing you to swing the leg around the...
Managing Fatigue with a Neurologic Condition
Fatigue is a major problem with a variety of neurologic conditions. Feeling fatigued can be a HUGE barrier in your physical recovery and it can also dramatically impact your overall quality of life.That being said, managing fatigue might be the single most important...
Movement Retraining when dealing with Spasticity
Spasticity is an involuntary muscle contraction due to damage to the brain or spinal cord. This can cause muscle stiffness and pain. Additionally, involuntary muscle contractions cause the body to move in ways that feel out of one’s control. This is turn can create...
Complete Guide to Buying a Wheelchair Cushion
Wheelchairs are an extremely valuable piece of equipment during the neurologic recovery process. They provide a means of getting around when walking is not safe and/or is not possible. However, they also come with the risk of developing pressure ulcers. Pressure...
Most Neglected Post Stroke Shoulder Exercise
Post stroke shoulder retraining often includes moving the arm bone. Unfortunately, many movement retraining programs fail to address the shoulder blade (flat bone on the back of the shoulder and the thoracic spine. Moving the humerus requires proper movement of the...