The Missing Link in Stroke Rehab: Why Strength Isn’t Enough
How Plyometric Exercises Can Improve Your Post-Stroke Walking
Recovering from a stroke is a journey that takes patience, effort, and persistence. Maybe you’ve been faithfully following your rehab plan—doing strength training, stretching, and walking drills
You might be hitting milestones in therapy, like improving walking speed and distance, but something still feels off. You may still feel a lack of confidence, especially when facing uneven surfaces, crowded spaces, or unfamiliar surroundings.
If this resonates with you, let’s talk about what might be missing from your recovery plan: plyometric exercises.
What Happens After a Stroke
After a stroke, it’s common to lose strength in one side of your body. But what many people don’t realize is that stroke impacts more than just strength.
That makes sense — weakness is often the most visible deficit. You might think, “If I just keep building strength, I’ll get back to normal.”
But here’s the truth: Strength is just one piece of the puzzle. What’s often overlooked is that your muscles do a lot more than contract. There’s coordination, muscle timing, power, and reflexive responses involved in nearly every movement — from stepping over a curb to reacting when you trip. That’s why you may still feel unsteady, even after regaining some strength.
So, What Are Plyometrics? 
Plyometric exercises train muscles to contract quickly after being stretched. This is known as the stretch-shortening cycle. Think of a rubber band: when you stretch it and let it go, it snaps back fast. That’s what we want our muscles to do!
In real life, this ability helps you react quickly and efficiently — like catching yourself from falling or adjusting to uneven ground — without overthinking.
Plyometrics are often used with elite athletes to build power, coordination, and injury resilience. Now, they’re being explored more in older adults to reduce fall risk. Yet in stroke rehab, they’re still largely missing — and that’s a problem.
Why Plyometrics Are Often Left Out of Stroke Rehab
There are a few reasons:
- Limited research: There’s still very little formal evidence on the use of plyometrics after stroke, especially for those with significant mobility impairments.
- Limiting beliefs in healthcare: Many therapists assume their patients can’t do these exercises, so they don’t even try.
- Misinterpretation of studies: Some studies labeled as “plyometric” actually just used fast sit-to-stands — which aren’t true plyometric movements.
Despite the lack of published evidence, clinical experience and anecdotal success show that these exercises can dramatically improve balance, confidence, and real-world function in stroke survivors — when used appropriately.
How to Safely Introduce Plyometrics After Stroke
If you’re thinking, “There’s no way I could jump or bounce,” don’t worry — there are many ways to scale plyometric movements to fit your current ability level.
Here are a few ideas:
1. TheraBand Recoil Drill
Attach a resistance band above your leg. Let it pull your leg upward, then push it down fast. This mimics the quick stretch/shortening cycle without putting weight on the leg.
2. Mini Trampoline Oscillations
With support (like parallel bars or a therapist), stand on a mini trampoline and gently bounce up and down — not jumping, just allowing your knees and ankles to absorb and release energy. This teaches coordination between the ankle, knee, and hip.
3. Assisted Pogo Jumps
Using a TheraBand for support, perform small jumps in place. You can start double-legged, then progress to staggered or single-leg positions for more challenge.
These movements not only improve muscle reaction time and coordination, but they also help rebuild the synergies between muscles — making movement more automatic and efficient.
⚠️ Important Note: Always do these exercises under the guidance of a trained therapist who understands how to scale movement based on your current mobility. Safety comes first.
Do You Need a Neurologic Physical Therapist?
Not necessarily.
In fact, some orthopedic physical therapists — especially those experienced with athletes or diverse age groups — may be more open to incorporating creative approaches like plyometrics. The key is finding someone willing to think outside the box and tailor therapy to your goals and abilities.
One Frustrating Example From Research
I recently found a 2025 study that seemed to confirm everything I’ve seen in practice. The conclusion supported the benefits of plyometrics in stroke recovery. Excited, I dove into the full article…
Only to find that the intervention wasn’t plyometric at all — it was just fast sit-to-stands. That’s not the same as tapping into the stretch-shortening cycle.
This highlights a bigger issue: Even peer-reviewed studies can miss the mark, and clinicians (and patients) often rely on conclusions without digging into the details.
Moral of the story: Ask for sources. Read studies for yourself. Understand whether the intervention tested applies to your situation.
Final Thoughts
Here are the 2 key takeaways:
- Plyometric exercises could be a critical missing link in stroke rehab — helping you move with more confidence, react faster, and reduce your fall risk.
- Your therapist’s beliefs matter. Don’t be afraid to ask questions, challenge assumptions, and seek care that aligns with your goals.
You have more potential than you’ve been told.
If you’ve had success (or struggles) with integrating advanced exercises like these into your rehab, I’d love to hear about it. Share your experience in the comments below — let’s build a stronger, more informed rehab community together.
Articles you may be interested in
Neuro Rehab is 90% mental, 10% physical
What should you expect to achieve in neurologic rehabilitation? My answer might confuse you, frustrate you, and hopefully challenge you to think differently. The most critical component of a successful outcome (in neurologic rehabilitation) is NOT based on the extent...
Hemiplegia: Fix a side bent trunk
Hemiplegia (weakness on one side of the body) can cause an unnatural "side bent" posture. This is sometimes also referred to as lateral trunk flexion. What is a "side bent" posture (lateral trunk flexion) with hemiplegia? A side bent posture is a “structural problem”...
Physical therapists are not as important as they think
I am not as important as I think I am. More broadly, physical therapists are NOT as important (to a rehab plan) as they may think. No, seriously. Ok, maybe half seriously. 2020 has been "unprecedented" (I couldn’t resist 🙃). I did what I thought I would never do....
Balance Training for Ataxia
Balance training is a critical component for anyone with ataxia. This is due to the fact that ataxia negatively impacts the balance system and is one of the leading causes of disability. Ataxia is caused by damage to the cerebellum. The cerebellum plays a MAJOR role...
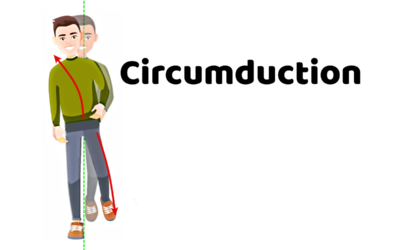
5 Problems that Lead to Circumduction
Circumduction is a “walking problem” that is characterized by the leg swinging out to the side. This is typically a compensatory strategy to prevent someone from catching the foot on the ground. Before we dive into what might be causing you to swing the leg around the...
Managing Fatigue with a Neurologic Condition
Fatigue is a major problem with a variety of neurologic conditions. Feeling fatigued can be a HUGE barrier in your physical recovery and it can also dramatically impact your overall quality of life.That being said, managing fatigue might be the single most important...
Movement Retraining when dealing with Spasticity
Spasticity is an involuntary muscle contraction due to damage to the brain or spinal cord. This can cause muscle stiffness and pain. Additionally, involuntary muscle contractions cause the body to move in ways that feel out of one’s control. This is turn can create...
Complete Guide to Buying a Wheelchair Cushion
Wheelchairs are an extremely valuable piece of equipment during the neurologic recovery process. They provide a means of getting around when walking is not safe and/or is not possible. However, they also come with the risk of developing pressure ulcers. Pressure...
Most Neglected Post Stroke Shoulder Exercise
Post stroke shoulder retraining often includes moving the arm bone. Unfortunately, many movement retraining programs fail to address the shoulder blade (flat bone on the back of the shoulder and the thoracic spine. Moving the humerus requires proper movement of the...
Relearn to walk: Progression (with videos)
Are you super eager to relearn to walk? Walking is a HUGE goal for anyone who has lost that ability. Walking means different things to different people. And quite honestly, has far less meaning until you have lost this fundamental skill. All that being said, it is...