You’ve Just Had a Stroke. Now What?
Acute Phase Recovery Guide – What to Expect in the First Few Days
First Things First…
If you’re here, you or someone you love has likely just had a stroke.
Let’s pause for a moment and say what most people won’t:
This is overwhelming.
The terms. The tests. The tubes. The questions. The uncertainty.
And yet, here you are—looking for answers, for help, for a path forward.
This article is for you.
What Is the Acute Phase of Stroke Recovery?
The acute phase is the very beginning—hours to days after a stroke. You’re still in the hospital (possibly the ICU), and things are changing fast.
At this stage, the brain is in crisis mode.
It’s working hard to protect itself, reroute signals, and begin healing.
During this time, you might experience:
- Confusion or difficulty communicating
- Weakness or paralysis on one side
- Vision changes, sensory loss, or trouble swallowing
- Emotional swings (tears, irritability, apathy—all normal)
- Fatigue and sleepiness
Good to know:
It’s often hard to tell how much function will return during this phase.
Some recovery may happen spontaneously over the next days and weeks. This is called “spontaneous neurological recovery.”
What Is a Stroke, Really?
In the simplest terms:
A stroke is a brain attack.
Blood flow to part of the brain was either blocked (ischemic) or disrupted by bleeding (hemorrhagic).
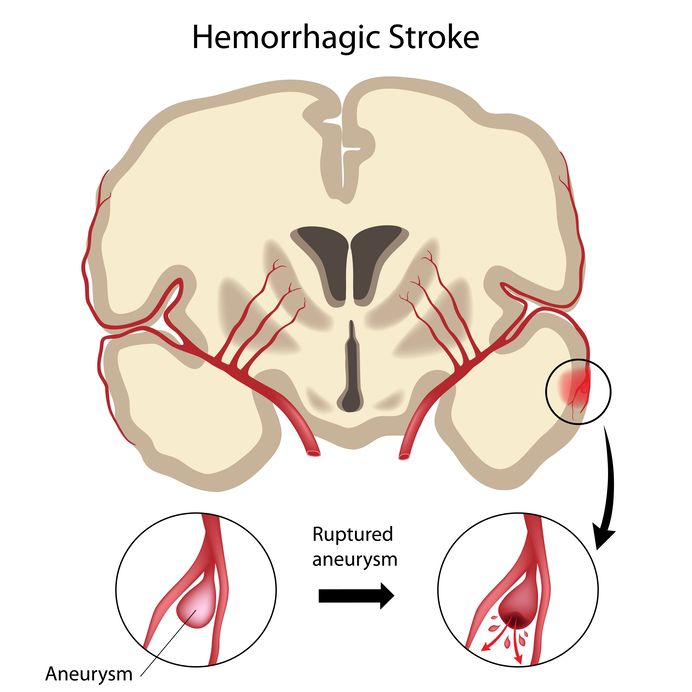
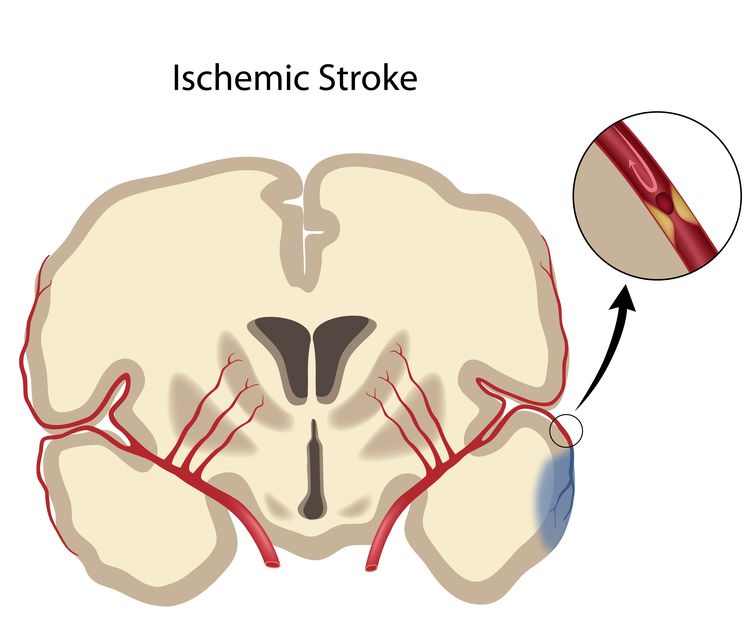
Without oxygen, brain cells in that area begin to shut down. That’s why time matters—and why emergency care is so critical in the first few hours.
Different areas of the brain control different functions—so symptoms and recovery will vary depending on where the stroke occurred.
What Happens Now?
You’ll likely go through the following steps:
1. Hospital Stabilization
- CT/MRI scans to locate the stroke
- Bloodwork and vitals monitoring
- Swallow study (to check for safety with eating)
- Medications to manage clotting, swelling, or blood pressure
2. Therapy Evaluations
- Physical Therapy (PT): mobility, strength, movement
- Occupational Therapy (OT): arm function, activities of daily living
- Speech Therapy (SLP): speech, swallowing, cognition
These early assessments help determine what kind of rehab you’ll need next.
What Can I Do to prepare for rehab?
Even in the hospital bed, there are things you can do to support recovery safely.
Here are a few safe activities you can do in your hospital bed (never start any activity without first talking to your medical team)
Sensory Activation
- Rub or tap the weak side of your body.
- Look at your affected hand and imagine it moving.
- Use a washcloth to gently stimulate the skin.
🧠 Why this matters:
Before movement comes back, the brain needs input. Sensory work tells your brain, “This part still matters.”
Passive Range of Motion
- Have a therapist or caregiver gently move your joints (shoulder, elbow, wrist, hip, knee, ankle). **Never move a family member who is in the hospital without first talking to the hospital medical team.
- Or guide your own weaker limb using your stronger arm.
🧠 Why this matters:
Movement—even if assisted—prevents stiffness and signals the brain that movement is still possible.
Breathing & Positioning
- Deep breathing helps with oxygenation and calming the nervous system.
- Change positions (with help) to avoid pressure sores and promote circulation. Again, NEVER move a family member who is in the hospital without first talking to the hospital medical team.
Why this matters:
Recovery isn’t just about limbs—it starts with core systems. Breathing well supports brain healing.
What Comes Next?
Within a few days, the hospital team will talk to you about:
- Inpatient rehab (3+ hours of therapy/day)
- Subacute rehab (less intensive but still daily)
- Home health or outpatient therapy (if medically stable)
Each path has pros and cons. Your medical team will consider your needs, support system, and overall condition.
If possible, ask for a family meeting with the rehab team before discharge so you can understand:
- Your current functional level
- What kind of recovery is expected
- What you should (and should not) do at home
Final Word
No one chooses this.
But you do get to choose how you respond.
Even if it feels like you can’t move.
Even if it feels like nothing is working.
Even if your brain is foggy and your body doesn’t feel like your own.
Something is happening.
Your brain is listening. And healing. And learning.
Start where you are.
Even if that means lying in a hospital bed doing deep breaths and tapping your arm.
That’s more valuable than you might think.
That’s the beginning.




